Bio-Technology, Cleanroom News, Contamination Control, DNA, FDA
Contamination Control vs Embryotoxicity
When you hear the phrase ‘designer babies,’ what springs most readily to mind? It’s an emotionally, socially, and politically loaded term that’s come to represent much of what’s ethically questionable in genetic research. Perhaps we might think of the movie Gattaca (that we referenced last week) in which genetics equal destiny. Or the 2003 German movie Blueprint, in which an incurably ill musician seeks to preserve her art by cloning herself to create a daughter who is simultaneously her child and her genetic twin. And of course, there’s always that early classic The Boys from Brazil (1978), in which a famous Nazi leader’s remains are used to create 94 replicas, with bioengineering as a tool of political and social control.
But that’s not all that cloning, genetic selection, bioengineering, and human genome sequencing research are about. Far from the pursuit of the perfect child, a next generation repository of talent, or the promise of a fascistic future, human genetic selection is more commonly used to promote fertility, prevent the transmission of disease, and eradicate terminal and incurable conditions. And nowhere is this more true and relevant than in the field of mitochondrial replacement therapy, or MRT.
We can tell we’ve piqued your interest, so what is MRT and why are we discussing it today?
Put simply, MRT is a potential answer to Mitochondrial Disease, a new family of disorders first defined in 1988. These conditions result from a failure of the mitochondria – the specialized part of every human cell (except for blood cells) that is responsible for generating energy. Sometimes referred to as intra-cellular powerhouses, the mitochondria create around 90% of the energy our organs require to sustain us. But recent research has demonstrated that this understanding of the function of mitochondria is an oversimplification, and it is a dangerous one at that. In fact, of the 3000 genes that are required to make a mitochondrion, only 3% of these are tasked with creating adenosine triphosphate (ATP), the nucleotide that transports chemical energy within a cell. So what do the remaining 97% of the genes do? Well, that depends on the cell they call home. If they happen to find themselves in the liver, they are in charge of detoxing ammonia in the urea cycle; in other cells, they may be responsible for hormone synthesis, the metabolism of cholesterol, or the oxidizing (breakdown) of our dietary macro-nutrients.
So given the enormous complexity of the human body, it is unsurprising that mitochondrial DNA serves a broad range of functions. And, by extension, it is also unsurprising that when it fails, the symptoms can run the gamut of problems. To wrap our minds around the problem, let’s give it a face – that of a 10-year old girl, Gina Mohan. Until the sudden and inexplicable onset of symptoms, Gina was just like any other ‘normal’ 10-year old. But when seizures left her unable to breathe, her family had little idea of the terrain of the territory it was entering. In a PBS NewsHour story published online by KQED, public radio for Northern California, Gina’s father, Chuck Mohan, reflected that ‘“There isn’t anything more frightening to a parent than to see a child in the middle of a seizure […] and there’s nothing you can do except wait for it to resolve.”’(1) In Gina’s case, four years of tests finally offered a diagnosis: mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes, or MELAS. And, as even the nomenclature suggests, mitochondrial diseases are not simple conditions: although they may have been present from birth, symptoms may remain dormant for years, striking apparently randomly and without warning. In Gina’s case, some of the seizures affected her diaphragm, and other sufferers also experience organ failure (particularly affecting tissues that have high energy demands such as the brain, liver and kidneys, or muscles such as the heart), exercise intolerance, blindness, and deafness.
Inherited via the maternal genetic line, the conditions are frequently unforeseen as some women can be asymptomatic carriers of the traits that will, overwhelmingly, lead to an offspring’s premature and inevitable death. As in Gina’s case, most mitochondrial disease cannot be cured and the only ‘treatment’ is initial prevention. Gina died from her illness eight months after her diagnosis, having just turned fifteen. Her father subsequently became the director of the United Mitochondrial Disease Foundation (UMDF), advocating for increased research testing and education in the field. Since our understanding of mitochondrial disease is not yet sufficient to develop cures, education is the premier tool in the fight to eradicate it. And by that we mean arming women with the information they need to make informed decisions – and this may include information on mitochondrial replacement therapy. So what is it and how does it work?
Already approved for use in in vitro fertilization (IVF) programs in the United Kingdom, MRT is also known – albeit erroneously – as the ‘three-parent baby’ solution, a term which makes medical professionals in the field bristle.
‘Mitochondrial donation’ might be a more accurate term for the process in which faulty inherited mitochondria are replaced with the healthy mitochondria of a donor. The nucleus of a fertilized egg is removed and is replaced by that of a donor egg, thereby implanting the fertilized egg with healthy mitochondria. The nuclear DNA, however, which contains 99.9% of genetic material from the mother and father, remains unchanged. So, although technically, the baby will have three sets of genetic material – maternal, paternal, and female donor – the relative dispersion is not equal.
So far, so good. Although the science is exciting, in relative terms it all seems comparatively straightforward and you’ll be forgiven for wondering where the controversy lies. Let’s take a broader look both at our own domestic situation and that of our international partners.
As it currently stands within the U. S., the federal Food and Drug Administration (FDA) is largely in opposition to mitochondrial donation and other mtDNA therapies.
However, overseas, other regulatory bodies are looking more favorably upon the science. In the United Kingdom, for instance, despite the perhaps inevitable opposition of the Catholic and Anglican Churches, MRT has been approved for use following an extensive survey of public opinion that found widespread support for additional research and patient access to the technology. The Human Fertilization and Embryology Authority (HFEA), the statutory, non-governmental body that oversees the regulation and inspection of all clinics engaged in IVF, artificial insemination, and egg/sperm/embryo storage, conducted the survey, presenting its findings to parliament which voted to permit both the practice of mitochondrial donation and the granting of licenses to clinics specializing in the practice.
And watching the developments in Britain, researchers in Singapore saw the potential for that country’s laws to change.
Under existing legislation, genetic manipulation was permissible in Singapore under the auspices of ‘research’ if done ‘formally as part of a study,’ noted Tracy Evans Chan, a review panel member for Singapore’s Bioethics Advisory Committee (BAC), the body responsible for advising the government on matters at the intersection of biomedical science and ethical-legal-social national frameworks.(2) Terming the procedure Mitochondrial Genome Replacement Technology (MGRT), the BAC issued a press release in April 2018 announcing a public consultation period ‘on the potential issues related to the clinical application of this emerging technology in humans.’(3) And interestingly this document touched very lightly on what has, here at home, became the Achilles Heel of the research: inheritance.
The extent to which genetic manipulation in one generation may result in changes in the next is an issue of grave concern to scientists and ethicists alike. Indeed, it was one of the questions for consideration in the BAC’s public comments solicitation in Singapore: ‘Should the welfare of future generations take precedence over the welfare of existing individuals (i.e. the prospective parents), or vice versa?’(4) In other words, are we justified in treating (or withholding treatment from) one generation knowing it will impact the next?
This is a thorny topic and one with which an expert panel convened by the U. S. National Academies of Science has been wrestling. Finding that within certain limitations MRT is considered to be both ethical and scientifically valid, the panel also reflected a strong concern about the potential for genetic manipulation. So on the one hand, approval was granted but on the other it did little to untie the regulatory hands of the FDA which ultimately was stymied in its attempts to permit the procedures. Why? Because, as the United Mitochondrial Research Foundation notes: “Despite this position, the FDA has been prevented from further evaluating clinical applications of MRT by language included in the 2016 congressional spending bill banning the agency from evaluating clinical trials involving genetic modifications that affect the next generation.” (our emphasis)
And so the debate continues…
But supposing the technology is ultimately approved here in the U. S. – what contamination control safeguards do we already have and how many more will we need to institute?
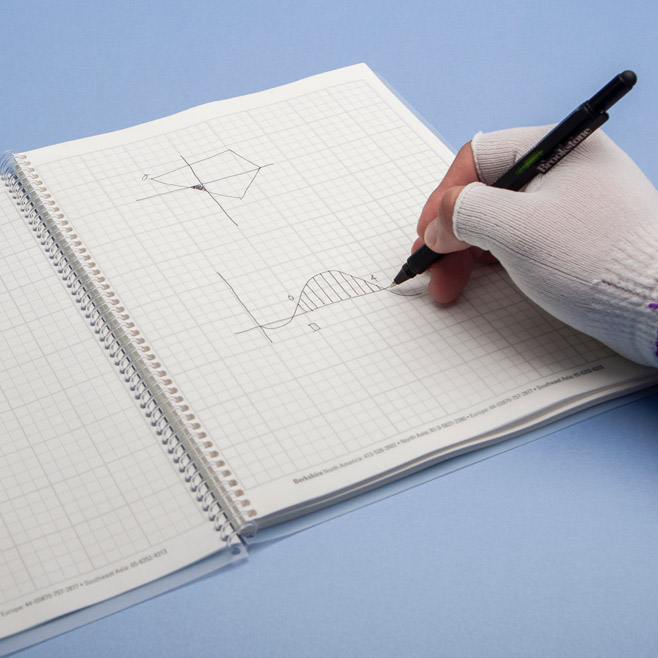
At this time, we do have a set of standard cGMPs and SOPs that relate to hospitals and other health care providers but IVF clinics and cryostorage facilities and cryopreservation locations require a whole extra level of care. We’ve written extensively on sterilization issues in hospitals, have investigated the ways in which the United Kingdom is raising the bar on IVF contamination control, and also have tackled the topic of tissue banks. But until now we haven’t paid much attention to the Cairo 2018 consensus on IVF laboratory environment and air quality: it’s time we remedied this omission. Published by Elsevier in its annals of Reproductive BioMedicine Online, the Cairo consensus is a proceedings report presenting the findings of an expert panel on the ‘recommended technical and operational requirements for air quality within modern assisted reproduction technology (ART) laboratories.’(5) And, despite its perhaps dry title, it is an interestingly comprehensive document. Ranging from how facilities should be constructed, to the design of heating, ventilation, and air conditioning systems, to the control of contamination and particulates (fungal, bacterial, and viral), and the presence of volatile organic compounds (VOCs), Cairo 2018 establishes more than fifty consensus points that the authors hope will be ‘aspirational benchmarks’ in the construction and maintenance of all ART labs.(6) And why is this so important? Because we are still largely at the cutting edge of the science and technology of human fertility and assisted reproduction with much to learn about the ways in which the environment affects embryonic gene expression and regulation. Inasmuch as we know the biology of the patients will influence gametes and potential embryos, we are increasing aware of the extent to which environmental factors also play a role, from contact with laboratory equipment to methodology, to cleaning materials and techniques. Let’s take a closer look at both of these last points…
Similarly some cleaning products contain ethanol which is an effective anti-microbial but also a VOC and known embryotoxin.
Cleaning materials. Chemically-based yet indispensible within any cleanroom environment. And yet the consensus for which to use in what circumstances is just that: a general idea but not a comprehensive set of guidelines. For instance, we know that cleaning agents containing chlorine dioxide (aka bleach) are wholly unsuited for use in IVF or ART facilities due to the concern for potential embryotoxicity. And yet bleach is extremely effective at killing spores – see ‘Disinfection of Cleanroom Surfaces with Bleach.’ Similarly some cleaning products contain ethanol which is an effective anti-microbial but also a VOC and known embryotoxin. And then there’s isopropyl alcohol, a chemical that should not be used in the presence of human tissues and yet pre-saturated wipes containing 70% IPA/30% Distilled water are a great choice for surface cleaning and the VOCs are minimized by the use of the wipe with its peel-and-reseal packaging. With that said, the IPA may also be replaced with an alcohol-free alternative that contains quaternary ammonium compounds or a simple 6% hydrogen peroxide solution. (For more information on the use of hydrogen peroxide, see our Learning Center article, ‘Disinfection of Cleanroom Surfaces with Hydrogen Peroxide.’
Cleaning techniques. There is also the question of the correct techniques to use.
As Rachel Cutting, principal embryologist and quality manager at the Center for Reproductive Medicine and Fertility Assisted Conception Unit at the Sheffield Teaching Hospitals NHS Trust in the UK, said in an article in Cleanroom Technology, where compromises are made on the chemicals used in IVF or ART environments, correct and efficient techniques become even more important: ‘Adapting cleanroom technologies to an IVF lab can be done – and over time, I believe more labs will change to this environment. It is a question of putting the right technologies, controls and processes into place – from filtering systems to culture media. Anything that can be done to stabilise (sic) the environment within an IVF lab must have a positive effect.’(7)
All of which leads us to wonder whether a refresher on the selection of appropriate cleaning materials and techniques is useful at this time. So far we’ve included links to our Learning Center articles where appropriate, and would also like to point readers to our articles on ‘Sources of Cleanroom Contamination’ for a general review of the key contaminants, ‘Q & A – Swab/Solvent Compatibility,’ for questions on pairing consumables with solvents, and ‘Cleaning a Contaminated Personnel’s Behavior – Decontamination Tools for Quality Managers,’ for assistance in tackling staff awareness with a diplomatic but effective approach to operator hygiene.
In addition, we’d also like to offer a quick reference to other points of consideration in an IVF or ART – or indeed any critical – environment:
- Personnel hygiene must be enforced: effective aseptic techniques demand adherence to strict hygiene regulations. Operators are known to be the #1 vector of contamination proliferation and every step must be taken to mitigate their potential for cross contamination. See our Learning Center article for a refresher on this issue.
- Cosmetics/Personal care products: while personal hygiene is critical (see above) operators should avoid the use of any products that could potentially release VOCs within the cleanroom environment. This would preclude the use of lotions, grooming products, perfumes, nail polish, or hand sanitizers, for instance, prior to entering a restricted area.
- Personal Protective Equipment (PPE) must be worn correctly – and donned correctly – at all times. This includes the use of hairnets, beard nets, masks, low particle-shedding clothing, and non-toxic, non-powdered gloves, as appropriate.
- Third-hand smoke: this is the smoke that enters a controlled environment on the hair or clothes of those exposed to second-hand smoke.
- Food, drinks, gum, etc must be avoided: anything that requires chewing or ingestion has no place within a cleanroom environment.
Some of these benchmarks may be new, or overlooked, concepts but others are standard and go back as far as the Institute of Environmental Sciences and Technology’s IEST-RP-CC027.2: Personnel Practices and Procedures in Cleanrooms and Controlled Environments.(8) But all of them should be part of a robust set of SOPs for any contamination-controlled environment.
The landscape for contamination control in the field of genetics/genomic research (and indeed in general) is evolving at a fast pace as technology continues to push towards the frontiers of what is possible. And with each advance in that technology, with each new technique that cultures life in embryonic form or that replaces damaged mitochondrial DNA we, as an industry, must be ready to raise the bar in our contamination control technologies accordingly. After all, the stakes, as any prospective parent will tell you, are high. Surely our industry bar for excellence in sterility should be even higher?
References:
- https://www.pbs.org/newshour/science/term-three-person-baby-makes-doctors-wince
- http://www.sciencemag.org/news/2018/06/singapore-could-become-second-country-legalize-mitochondrial-replacement-therapy
- http://www.bioethics-singapore.org/images/uploadfile/BAC%20MGRT%20Press%20Release.pdf
- ibid
- https://www.sciencedirect.com/science/article/pii/S1472648318300890
- ibid
- https://www.cleanroomtechnology.com/technical/article_page/Fertile_ground_for_cleanrooms/51529
- http://www.iest.org/Standards-RPs/Recommended-Practices/IEST-RP-CC027


















HAVE AN IDEA FOR CONTENT?
We are always looking for ideas and topics to write about.
Contact Us